Diabetes is a chronic condition characterized by an impaired ability to regulate blood sugars.
The Public Agency of Canada (2023) has found that 10% of individuals in Canada are diagnosed with diabetes, with 90-95% of cases being Type 2 diabetes.
Moreover, 6% of individuals 20-79 years old in Canada live with pre-diabetes, defined by having elevated blood sugar levels that fall just below the threshold of a diabetes diagnosis.
Dealing with diabetes, whether personal or that of a loved one, can be a stressful and emotional experience. Here are some diabetes basics to help build your understanding.
What is the difference between Type 1 and Type 2 Diabetes?
Type 1 diabetes is an autoimmune condition where the body attacks its own beta cells in the pancreas.
Beta cells are primarily responsible for the production of insulin, the hormone that helps lower blood sugar. Thus, the body is unable to produce insulin on its own and must rely on exogenous (external) insulin to regulate blood sugar.
Type 2 diabetes is a metabolic condition where the body has an impaired response to insulin or the body produces inadequate amounts of insulin.
The initial intervention for type 2 diabetes is usually lifestyle changes via diet and physical activity. If blood sugars are still outside the ideal range, medications may be suggested by your healthcare provider to further support blood sugar control.
Gestational Diabetes (GDM) develops during pregnancy due to hormonal changes and affects about 10% of women who give birth. Learn more about GDM here.
Common Signs and Symptoms of Diabetes
When blood sugars are high for extended periods of time, people can start to develop symptoms such as the following:
- Extreme thirst
- Frequent need to pee
- Unexplained weight changes (gain or loss)
- Extreme fatigue or lack of energy
- Slow healing wounds and/or recurrent infections
These symptoms may develop within a few weeks or take months to years to be noticed.
It is also possible to have no obvious symptoms and have diabetes. It is recommended you contact your doctor if you suspect you or a loved one may have diabetes.
Understanding Your Diabetes Numbers
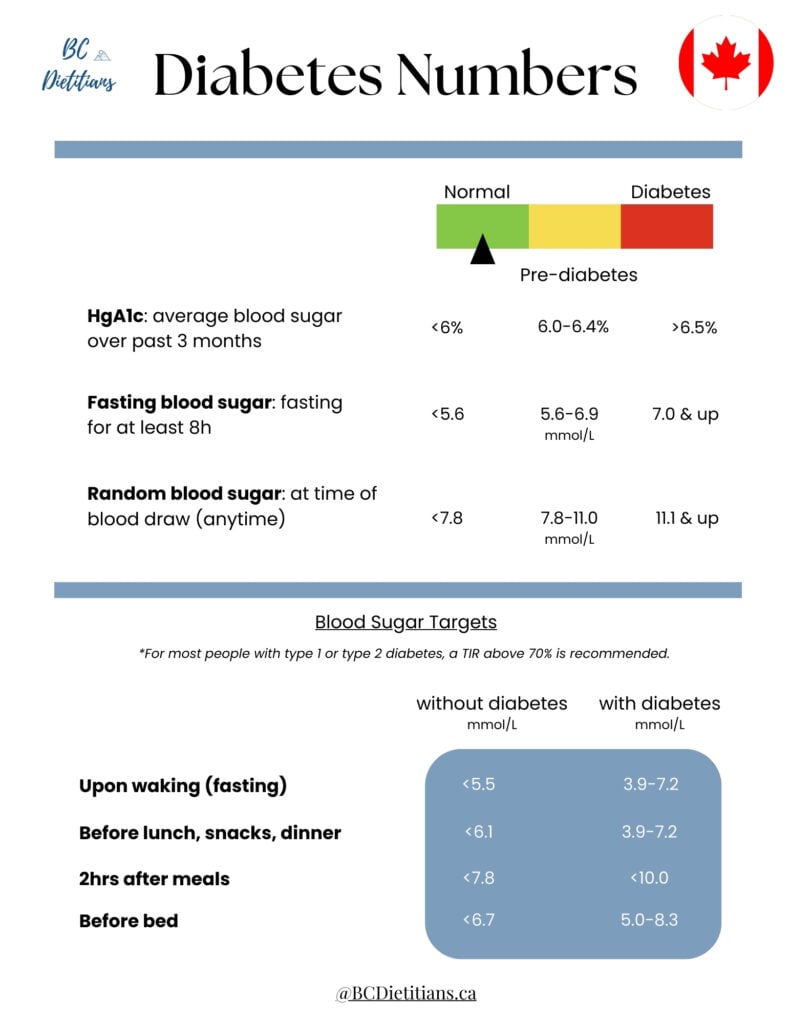
Hemoglobin A1c
Hemoglobin A1c (HgA1c or A1c test) is a blood marker that estimates your average blood glucose levels over the past 3 months.
This test does not need to be done fasted as it measures average blood sugar levels and not specific levels at the time of blood drawing.
- Normal range: <6.0%
- Pre-diabetes; increased risk of developing diabetes: 6.0-6.4%
- Diabetes: 6.5% and up
For those curious: How does this test estimate blood sugars in the past 3 months?
When sugar levels in the blood are high, there is an increased likelihood of the sugars sticking (glycating) to the red blood cells in the blood.
This test measures the percentage of red blood cells that have sugar stuck (glycated) to them. Since red blood cells have a lifespan of 2-3 months, this test offers insight into your average blood sugars in the past 3 months.
Fasting Blood Glucose
This test must be done fasted, meaning no food or drinks (with the exception of water) for at least 8 hours before the blood draw. A result of 7.0mmol/L or greater can be an indicator of diabetes.
Random Blood Glucose
This test measures the amount of glucose in your blood at the specific time of blood draw. This test does not require you to be fasted prior to drawing blood.
A reading of 11.1 mmol/L or higher can be an indicator of diabetes but factors such as other symptoms of diabetes also need to be considered.
Diabetes Risk Factors
There are several factors that can affect your risk of developing diabetes. Some factors that predispose you to diabetes are out of your control such as sex, age, genetics, and ethnicity.
However, there are also many factors in your control that can help decrease your risk of developing diabetes.
Risk Factors you can’t change :
Sex
- males are at increased risk of developing type 2 diabetes
Age
- your risk of developing diabetes increases as you age
Genetics
- you may have an elevated risk of developing diabetes if you have family members who have diabetes. In addition to genetics, families may also share lifestyle factors that increase diabetes risk
Ethnicity
- People of African, Arab, Asian, Hispanic, Indigenous, and South Asian descent may have an increased risk of developing type 2 diabetes
Risk Factors you can change:
Weight:
- maintaining a healthy weight decreases your risk of diabetes
Waist circumference
- increased body fat around the abdomen is a risk factor for developing type 2 diabetes. A healthy waist circumference is <102cm for males and <88cm for females
Physical activity
- Engaging is an average of 30 minutes of movement per day or 150 minutes per week decreases your risk of developing type 2 diabetes
Fruits and vegetable intake
- Increase your intake of foods rich in fiber and reduce your intake of fat and salt. It is recommended to consume 7-10 servings of fruits and vegetables a day
Blood pressure
- High blood pressure is a risk factor for developing type 2 diabetes.
Decrease your risk of high blood pressure through regular movement, reducing salt and fat in your diet, limiting alcohol consumption, avoiding smoking, and maintaining a healthy body weight.
How do you check your blood sugar?
There are 2 main ways people test their blood sugar levels at home.
The traditional method is using a finger prick – people use a lancet to prick their finger, then transfer the drop of blood onto a blood glucose monitor. The monitor is able to analyze the glucose level from the blood in less than a minute.
The advantages of finger-prick blood glucose monitors include:
- Requires less use of technology, making it more suitable for people who are less technologically savvy like seniors
- Is often the more affordable option
A newer method of testing blood sugar is through continuous glucose monitoring (CGM) devices.
These devices attach to the skin, with sensors lasting 7-14 days, depending on the brand of device. They read glucose levels via a thread that sits right below the skin of the person. The thread is as small as a single soft toothbrush bristle or thin hair.
The advantages of CGMs include:
- Providing continuous data that allows you and your provider to track a full day’s blood sugar trend
- Evidence-based technology that can help improve your blood sugars due to the instant feedback
- Does not involve daily finger pricking, which can increase risk of infection and cause soreness around the finger tips
- Can alert you of high and low blood sugar events as they happen
Diabetes Canada has compiled this in-depth resource highlighting the benefits, limitations, and costs of the different glucose monitoring methods.
How often should I check my blood sugar?
How often you need to check your blood sugar depends on whether you have type 1 or type 2 diabetes, whether you take insulin, the variability in your schedule, and your overall health.
Always default to your healthcare provider’s advice.
General recommendations are to check your blood sugar:
Upon waking or before breakfast
- Indicates your fasting blood glucose
- Goal range for people with diabetes: 3.9-7.2 mmol/L
Before meals and 2 hours after meals (especially the biggest meal of the day)
- Indicates if your body is producing enough insulin for the food you’re eating
- It could also be helpful to keep a food log of what and how much you ate for each meal and snack to understand how your intake is affecting your blood sugar
- Goal range for people with diabetes before meals: 3.9-7.2 mool/L
- Goal range for people with diabetes 2hrs after meals: <10 mmol/L
Before bed
- Identifies if your blood sugars are within range before bed
- Goal range for people with diabetes: 5.0-8.3 mmol/L
If you use a blood glucose monitoring device, you do not need to worry about checking your blood sugar at specific times of the day as the device will graph this for you.
You may still have to hold your phone next to monitor for it to sync the data depending on the specific device you have.
Your doctor or dietitian may recommend you fill out a food and activity diary for a few days to get a better picture of your blood sugars throughout the day. Here is an example of a food and activity diary template.
A diary helps you and your provider link your blood sugar readings to the timing of your intake and activity, allowing them to better recommend changes as needed.
If you use a glucose monitoring device, you may be able to log your intake and activity via the device’s app.
What can I do to improve my blood sugars with Diabetes?
Eat 3 meals per day at regular times
- Eating at regular times helps your body control blood sugars
- Space meals no more than 6 hours apart
- For snacks, always pair your carbohydrate with a protein and/or healthy fat source
Limit sugars and sweets
- Simple sugars cause spikes in your blood sugars
- Limit your intake of free sugars to <5-10% of your total daily calorie intake.
This is approximately 26-50 grams (6-12 teaspoons) of free sugars based based on a 2000kcal diet. Free sugars refers to added sugars.
Eat more high fiber foods
- Fiber helps maintain satiety and slows digestion, allowing for a slower, controlled rise in blood sugar.
- Opt for carbohydrates with fiber. Choose whole-grain alternatives over processed and white carbohydrates
- Adults should aim for 25-38g of fiber per day
Opt for water
- Sweetened drinks like regular pop is a common source of added sugars
- Bring a water bottle with you when you go out or go to work
- Carbonated water and tea without added sugars can be good alternatives
- Adults should aim for 2.7-3.7L of water per day
Move your body regularly
- Physical activity helps improve your blood sugar control
- Adults should aim to engage in an average of 150 minutes of moderate to vigorous physical activity a week (average of 30 minutes, 5 days a week)
- A good way to start is incorporating a 10 minute walk after meals
Avoid/Limit drinking alcohol
- Alcohol may cause low blood sugar events and cause weight gain
Take your diabetes medication(s) as recommended by your doctor
- Poorly controlled blood sugars can lead to serious complications such as kidney damage, eye damage, nerve damage, and poor healing wounds
- If you use any supplements to manage your diabetes, be sure to discuss this with your doctor. We have previously completed a comprehensive review on these popular supplements for blood sugar control
Book a dietitian consultation with a certified diabetes educator
- A dietitian trained in diabetes education can help identify exactly what you need to do to help manage your blood sugars
- A registered dietitian can help you take control of your diabetes by creating a personalized eating plan that supports stable blood sugar levels, fits your lifestyle, and includes your favorite foods
- They also provide ongoing support, education, and guidance to prevent complications and promote long-term health
Key Takeaways
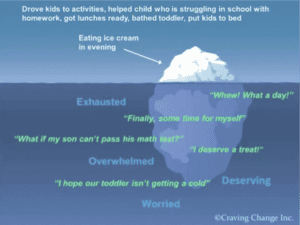
Blood sugar control is influenced by many factors including diet, exercise, stress, hormones, illness, medications, sleep, and alcohol.
It can sometimes be a frustrating journey to navigate, especially if you have a new diagnosis, or if your blood sugar pattern has suddenly changed after finding a regimen that worked for you.
Here are some questions to reflect on and discuss with your doctor or dietitian:
- What strategies have been working well for you?
- What strategies have you already tried?
- What strategies do you think might work? Or what are you currently doing that you think could be done differently?
- Do you notice any patterns in your blood sugars (highs or lows) throughout the day or week?
- What other factors have changed in your life that may be affecting your blood sugar control?
Blog Contributors:
Amy Chow, Registered Dietitian
Kelly Chia, Dietetics Student
References :
- Public Health Agency of Canada. (2023). A snapshot of diabetes in Canada. Retrieved from https://www.canada.ca/en/public-health/services/publications/diseases-conditions/snapshot-diabetes-canada-2023.html
- Diabetes Canada. (n.d.). Diabetes 360° and ethnic high-risk populations. Retrieved from https://www.diabetes.ca/DiabetesCanadaWebsite/media/Advocacy-and-Policy/Diabetes-360-and-ethnic-high-risk-populations.pdf
- Government of Canada. (n.d.). CANRISK: Diabetes risk questionnaire. Retrieved from https://www.healthycanadians.gc.ca/en/canrisk
- Diabetes Canada. (n.d.). Alcohol and diabetes. Retrieved from https://www.diabetes.ca/DiabetesCanadaWebsite/media/Managing-My-Diabetes/Tools%20and%20Resources/alcohol-and-diabetes.pdf
- Diabetes Canada. (n.d.). Exercise and activity. Retrieved from https://www.diabetes.ca/nutrition-fitness/exercise-activity
- Diabetes Canada. (n.d.). Sugar and diabetes: Our policy position. Retrieved from https://www.diabetes.ca/advocacy—policies/our-policy-positions/sugar—diabetes
- Diabetes Canada. (n.d.). Symptoms of type 2 diabetes. Retrieved from https://www.diabetes.ca/about-diabetes/type-2/symptoms
- University Health Network. (n.d.). My Food Diary – Keeping track if you have diabetes. Retrieved from https://www.healtheuniversity.ca/EN/CardiacCollege/Stroke/Documents/LT_m_My_Food_Diary_(Keeping_track_if_you_have_Diabetes).pdf
- Dexcom. (n.d.). What are normal blood glucose levels? Retrieved from https://www.dexcom.com/en-CA/faqs/what-are-normal-blood-glucose-levels



Add a comment