Menopause and perimenopause are big life changes – physically, emotionally, and socially. While hot flashes get all the attention, there may be other symptoms that you have been experiencing like weight gain, brain fog, and low energy. Menopause doesn’t just affect how you feel, this new phase in your life can have a huge impact on your long-term health.
- How to Know If You’re in Perimenopause
- Hormone Replacement Therapy
- Lifestyle Changes to Manage Menopause Symptoms
- How Menopause Changes Your Nutrition Needs
- Supplement Considerations in Menopause
- Do I Need More Protein During Menopause?
- Is Perimenopause Weight Gain Inevitable?
- Personalized Nutrition in Midlife = Less Stress, More Energy
How to Know If You’re in Perimenopause
Perimenopause is the transition period to menopause, and menopause is reached after 12 consecutive months without a period, typically between 46 and 55 years old. This often lasts for several years, and can happen earlier than expected for some women. 3% of women may experience premature menopause before the age of 40.
In perimenopause, estrogen and progesterone begin to decrease, and follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels start to increase.
The hormone fluctuations may contribute to these common signs of perimenopause:
- Migraines: Changes in estrogen and progesterone affects neurotransmitters and pain networks in the body, affecting the frequency and severity of migraines.
- Changes in menstrual flow and frequency
- Hot flashes and night sweats – Sudden, intense sensation of heat in the upper body: Declining estrogen levels affect the hypothalamus, and subsequently heat regulation.
- Changes in mood – Feeling more depressed and sensitive to stress: Declines in estrogen and progesterone disrupt neurotransmitters like serotonin and norepinephrine, which play a key role in regulating mood. Poor sleep is also a contributing factor.
- Brain fog – forgets things easily and have trouble focusing: estrogen plays a role in cognition and memory, and declining estrogen levels may lead to decreased neuron firing and energy levels in the brain.
- Frozen shoulder – related to decreasing estrogen levels which can lead to increased inflammation and tissue changes. Other underlying health conditions such as diabetes and elevated triglycerides can lead to fatty deposits build up in the arteries, further contributing to frozen shoulder.
- Hair loss – decline in estrogen and progesterone can decrease the hair’s growth phase and lead to slower hair growth. Other contributing factors include genetics, nutrient deficiencies, and stress.

Hormone Replacement Therapy
Menopausal Hormone Replacement Therapy (HRT) is a treatment that adds back estrogen and progesterone to help reduce symptoms such as hot flashes, night sweats, and mood swings. It can also support bone health.
HRT isn’t right for every woman, and long term use may slightly increase the risk of some health conditions, including heart disease and some types of cancers.
Starting March 2026, BC will offer free coverage of HRT to treat menopausal symptoms. It’s important to talk with your doctor about whether it’s a good option for you, and to assess benefits and risks in relation to factors such as your age and the year of menopause onset.
Lifestyle Changes to Manage Menopause Symptoms
Nutrition and lifestyle changes can still play a big role, whether or not you are using HRT.
While nutrition alone won’t “cure” these symptoms, certain dietary choices may help reduce frequency and/or intensity. No food can single-handedly balance hormones, but it can support your body’s natural hormonal regulation when paired with adequate sleep, stress management, and physical activity.
Soy and flax seeds are also commonly used to manage symptoms like hot flashes. Current evidence shows some potential in incorporating these dietary recommendations for menopausal symptoms, but more consistent data is needed.
Reducing triggers such as alcohol, caffeine, and spicy foods can help with hot flashes, along with maintaining a healthy weight.
A MSCP dietitian understands the complex hormonal changes during perimenopause and can help you navigate this new life stage with a tailored nutrition plan based on the latest evidence.
How Menopause Changes Your Nutrition Needs
Shifting hormones in the menopause transition can increase your risk of heart disease, osteoporosis, and even mental health challenges.
Hot Flashes and Night sweats = Links to Chronic Diseases?
Emerging research shows frequent or severe VMS during menopause may indicate a higher risk of developing cardiovascular disease, metabolic syndrome, diabetes, fatty liver, and osteoporosis.
Inflammation, vascular dysfunction, and changes in thermoregulation may be related to the chronic diseases and affect the severity of these symptoms.
As your body is undergoing these changes, it is the perfect time to look into your nutrition and lifestyle. Nutrition plays a powerful role in supporting good health for the next couple decades of your life.
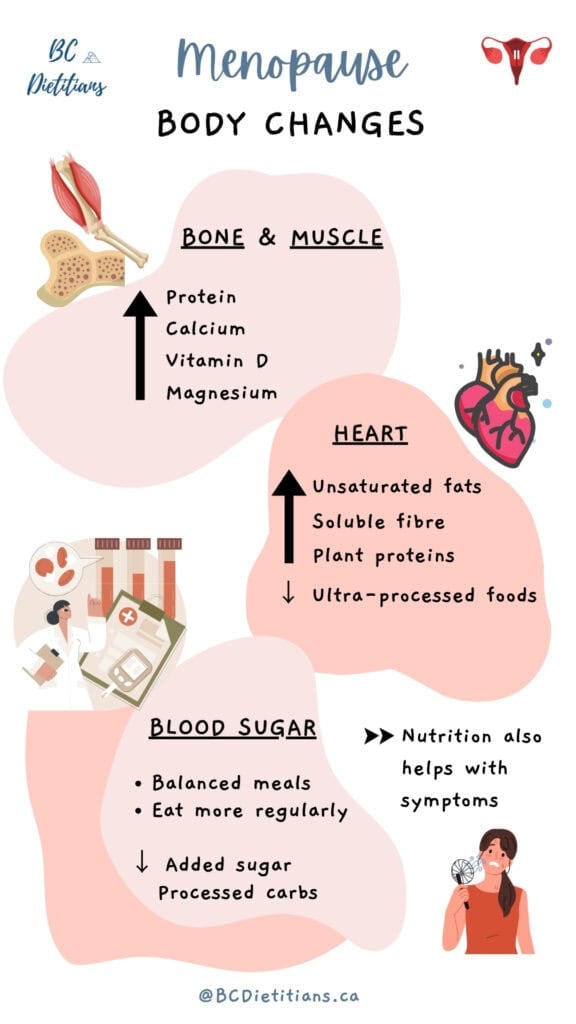
Bone and Muscle Health
Estrogen plays a key role in maintaining strong bones. When it drops, calcium absorption decreases, and bone breakdown speeds up. 50% of postmenopausal women will develop osteoporosis, a condition that weakens your bones over time, and increases the chances of fractures.
Research indicates that we can lose up to 20% bone mass during perimenopause and the few years after. Muscle loss can also happen during this time, both due to aging and the decline in estrogen, which plays a role in muscle repair and regeneration. That’s why nutrients like calcium, vitamin D, magnesium, and protein become so important.
Key nutrition strategies:
- Calcium-rich foods (dairy, tofu, leafy greens, fortified plant milks): Calcium is one of the main minerals in bones. If you don’t get enough through food, your body pulls it from your bones, which weakens them over time.
- Get enough vitamin D (sunlight, food, supplements): Vitamin D helps with calcium absorption. Together, Calcium and vitamin D enhance bone formation and prevent fractures.
- Eat enough magnesium (avocados, black beans, seeds, and whole grains): These support bone structure and help activate vitamin D. About 60% of total body magnesium is stored in the bone.
- Eat enough protein: Protein is the building block for bone and muscle. Eating enough helps maintain bone density and prevents muscle loss, especially when combined with strength training.
Heart Health
Estrogen helps to maintain healthy cholesterol levels and protects your heart before menopause. But when your estrogen levels drop during menopause, the risk of high cholesterol increases and your heart may become more vulnerable to heart disease.
Women are 5x more likely to die of cardiovascular disease than breast cancer. Heart disease is the #1 preventable cause of death among Canadian women.
Key nutrition strategies that can help protect your heart:
- Focus on unsaturated fats (olive oil, avocado, nuts, seeds, fatty fish): These fats can help lower LDL cholesterol and support healthy blood vessels.
- Add omega-3s (salmon, chia seeds): Enough dietary omega-3s can play roles in reducing inflammation and risk factors for heart disease, including blood pressure and triglyceride levels.
- Include soluble fiber (oats, flaxseed, beans): These help lower LDL cholesterol.
- Reduce intake of added sugars and ultra-processed foods: These can raise triglycerides and contribute to inflammation.
- Include plant-based protein: Plant-based proteins can lower LDL cholesterol and reduce the risk of heart disease in some people.
Blood Sugar
Low estrogen levels may increase fasting blood sugar and decrease insulin sensitivity, making your blood sugar more likely to spike and crash.
This can lead to:
- Increased cravings
- Low energy or “crashes” after meals
- A higher risk of developing insulin resistance or type 2 diabetes
Key nutrition strategies that can help stabilize your blood sugars:
- Eat regular, balanced meals with protein, fiber, and healthy fats to prevent dips in energy and stabilize blood sugar.
- Limit highly processed carbs and sugary foods: These can lead to blood sugar spikes and crashes because they are lower in fiber and are absorbed quickly.
- Focus on low-glycemic whole foods (beans, vegetables, and whole grains): These are digested more slowly, and leads to a slower rise in blood sugar levels. This helps with blood sugar control and prevent sharp increases in insulin.
Gut Health
Some women notice more GI symptoms such as bloating, gas, constipation, or irregular digestion during perimenopause. This can be due to shifting hormone levels, which affect digestion and the makeup of gut bacteria.
Key nutrition strategies to support gut health:
- Eat enough fiber: These can be from a variety of plant foods like fruits, vegetables, beans, nuts, seeds, and whole grains. They help keep digestion regular and feed healthy gut bacteria.
- Stay hydrated: Hydration helps with digestion and symptoms like bloating.
- Limit ultra-processed foods, added sugars, and alcohol: These can negatively affect gut bacteria and worsen symptoms.
- Eat slowly and mindfully: These habits help reduce symptoms such as gas and bloating.
Supplement Considerations in Menopause
For some women, supplements may be useful in addition to a balanced diet, especially if blood work and/or dietary intake shows a need. It’s always important to consult your healthcare provider before starting any new supplement.
B vitamins: These are important for brain health, heart health, energy and protein metabolism. Health Canada recommends adults over the age of 50 get most of the vitamin B12 from synthetic sources (fortified food or supplement).
Vitamin D, calcium, magnesium, and protein: These nutrients are critical for bone and muscle health, amongst their other roles.
Health Canada recommends all adults over the age of 50 take 400 IU vitamin D supplements daily. If you can’t meet your calcium needs through food alone, you can consider taking a daily supplement containing 500mg calcium to help meet the recommended 1200mg intake per day.
Protein powders (generally 1 scoop, or 25-30g, per day) can be used to help meet your daily protein needs, if it can’t be met with food alone.
Magnesium is abundant in plant foods, but supplements of generally no more than 350mg magnesium per day may be recommended – particularly for severe menopausal symptoms (e.g. migraines) or if there is a deficiency.
DHEA (dehydroepiandrosterone): This is a hormone used by the body to make estrogen, and its level decreases during menopause. DHEA deficiency can also affect bone density. A blood test can decide whether DHEA supplement is needed, with typical dosage starting at 25-50mg per day. This should be taken under medical supervision because DHEA affects the levels of other hormones in the body ie. testosterone.
Omega-3s, namely eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), have anti-inflammatory properties and help support heart health. Supplementation with 1-3g per day of EPA and DHA per day may be recommended for vegetarians and vegans, who may find it challenging to get enough from food alone. Supplementing with 600-650 mg of EPA and DHA may be sufficient for women who eat fish twice a week.
Inositol (1-4g daily) and ashwagandha (up to 1000 mg daily) may offer benefits for stress relief and managing cortisol levels when paired with other stress management tools including movement, and nutrition. Inositol may also offer some benefits for women with PCOS, diabetes, and may help support metabolic health and weight changes.
Do I Need More Protein During Menopause?
With high-protein diets trending in the wellness world right now, it’s important to remember that our protein needs are highly personal – they are based on factors such as body size, activity level, and health status.
During perimenopause and postmenopause, protein is especially critical for:
- Maintaining muscle mass and bone health
- Stabilizing blood sugar levels
- Reducing cravings and energy crashes
- Helping to lower cholesterol and blood pressure (especially with nutrients like magnesium and fibre from plant-based proteins), thereby lowering the risk of heart disease
Research suggests a daily protein intake of 1.4-2.2g per kg body weight. If you’re an athlete or very active, it may be a good idea to aim for the higher end of that range to support muscle and recovery nutrition.
For a simple starting point, most healthy adults going through the menopause transition can benefit from getting 25-30 grams of protein at each meal.

Is Perimenopause Weight Gain Inevitable?
Weight and body shape changes during perimenopause are one of the most common concerns I hear from my clients.
Weight is an outcome of many factors. Some factors are independent of menopause – for example, genetics, normal aging and life situations and stress.
Weight gain in menopause may be more common because of:
- Hormonal changes: A drop in estrogen can lead to the redistribution of fat, increased fat storage around the midsection, and loss of muscle mass.
- Poor sleep: Low progesterone and estrogen levels can cause symptoms like night sweats and negatively impact sleep quality. Poor sleep can interfere with the normal functioning of hormones that regulate hunger and fullness, leading to changes in eating patterns. Lack of sleep can also negatively affect energy expenditure, metabolism, and increase risk of chronic health conditions.
- Mental health: Mood changes like depression can lead to stress eating, which could mean increased cravings and caloric intake for some.
Staying on top of your weight can feel like an impossible task at this time.
It’s important to remember that your weight does not determine your health, and you can improve your health, energy, and well-being independent of weight loss.
Let’s shift the focus from “How do I lose weight?” to “How do I feel strong, nourished, and supported?”
Start with sustainable habits:
- Joyful, consistent movement
- Balanced eating patterns with nutrient-dense foods
- Prioritizing sleep and stress management
- Kindness and patience with your changing body, and focus on what feels good for you
Many of my clients wonder if intermittent fasting can help them tackle the unwanted menopause weight gain. Intermittent fasting is no different than other forms of caloric restriction, and it is no more effective than any other diet in achieving weight loss.
For many women, especially during this phase of life, intermittent fasting is often unhelpful and can backfire – it may increase fatigue, blood sugar instability, or emotional eating.
Instead of restricting and adding on more food rules, I work with my clients on an eating pattern that is satisfying, nourishing, and sustainable so you can enjoy and thrive at this stage of your life.
Personalized Nutrition in Midlife = Less Stress, More Energy
Menopause shouldn’t have to feel miserable. With the right support, you can feel stronger, clearer, and more in control of your health than ever before.
Working with a MSCP dietitian can help you:
- Gain energy and fight fatigue (by addressing things like iron levels and eating patterns)
- Protect your bones and heart with the right nutrients at the right time
- Let go of dieting – and regain your health and freedom
- Avoid wasting time, money, and energy on the wrong “solutions”
You deserve support that respects your body.
There’s no perfect time to start improving your health. Just the right time for you.
Connect with me at The Nourished Menopause for guidance you can trust and support that meets you where you are.





Add a comment