In the recent years, GLP-1 (glucagon-like peptide-1) medications such as Ozempic, Wegovy, Rybelsus*(oral semaglutide), Mounjaro* (a dual agonist that mimics both hormones – GLP-1 and GIP) have rapidly gained popularity in recent years, especially among those managing their weight or dealing with Type 2 diabetes. The global GLP-1 market is forecasted to exceed $100 billion by 2030, driven by both diabetes and obesity treatment needs and the effectiveness of these medications in regulating blood sugar and appetite.7
GLP-1 medications have made it onto the list of the top ten food and nutrition trends in 2025. But what exactly is GLP-1, how does it work in the body, and why should you care about it? In this post, we’ll break down the science behind GLP-1 medications, explore the common side effects you should consider, and highlight the importance of personalized nutrition in optimizing their benefits.
What is GLP-1?
GLP-1 is a hormone naturally produced in our body. It plays a significant role in regulating blood sugar levels and appetite. After eating, GLP-1 helps stimulate insulin secretion when blood sugar is high and helps cells absorb sugar from the blood. It also suppresses glucagon (a hormone that increases blood sugar), slows down gastric emptying, contributing to feeling full after meals and reducing hunger.
GLP-1 receptor agonists are medications that mimic the natural hormone GLP-1’s effects to help people with Type 2 diabetes and/or weight loss in overweight adults. Semaglutide meds include Wegovy which is specifically approved and marketed for weight loss, and Ozempic, which is primarily approved and prescribed for the treatment of type 2 diabetes (with the off label use for weight loss).
Questions to Ask Your Doctor
Anyone considering starting GLP-1 medications should have a clear understanding of the medication, its potential benefits, and possible risks. Here are some essential questions to ask your doctor so you can make an informed decision:
- Am I a good candidate for GLP-1 therapy based on my health conditions?
- What are the potential benefits and side effects of GLP-1 medications?
- What are the options and costs associated with these medications?
- Are there any interactions with other medications I am taking?
- What lifestyle changes should I make while on GLP-1 therapy?
- Are there any long-term concerns I should be aware of?
- What should I do if I miss a dose or experience side effects?
- How often will I need to follow-up while on GLP-1?
- Can GLP-1 therapy be used long-term? How long would I be on this medication?
These questions will help empower you to have informed discussions with your healthcare providers about GLP-1 therapy, ensuring you make well-considered decisions for your health and personal goals.
Who Should Not Use GLP-1?
GLP-1 medications may be contraindicated if you have or have a history of:
- personal and family history of papillary and follicular thyroid
cancers (given that there may be an increased risk based on animal studies) - chronic nausea, vomiting or gastroparesis (as GLP-1s slow down gastric emptying and may worsen GI symptoms)
- Pancreatitis (GLP-1s may increase the risk of pancreatitis or inflammation of the pancreas)
- currently pregnant or breastfeeding
- eating disorders
- allergy or hypersensitivity to the medication
Always consult a healthcare professional before starting GLP-1 medications to ensure they align with your health needs and treatment plan. A personalized assessment will help determine if GLP-1 is the right option for you based on your specific health conditions, medical history, and treatment goals.
How Does GLP-1 Work in the Body, and Who May Benefit?
GLP-1 medications, such as Ozempic, Wegovy and Mounjaro, are now prescribed commonly for people diagnosed with Type 2 diabetes and/or obesity. These medications are effective at managing blood sugar levels and supporting weight loss, making them beneficial for certain health conditions. Studies show that GLP-1 medications are effective for both Type 2 diabetes and obesity treatment, helping with weight loss and blood sugar control.
Your doctor will prescribe Wegovy based on the following dosing schedule:
- 0.25mg, once a week for 4 weeks
- then increased to 0.50mg, once a week for 4 weeks
- then increase to 1.0mg, once a week for 4 weeks
- then increase to 1.7mg, maintain dosage once a week afterwards
- OR may continue increase to 2.4mg, maintain dosage once a week afterwards
GLP-1 medications mimic the effects of the naturally occurring GLP-1 hormone in the body, which plays a crucial role in regulating blood sugar and appetite. GLP-1 hormone plays an important role in both glycemic control and weight loss.
We break down how these medications work and who may benefit most from them:
1. Regulates Blood Sugar
For people with Type 2 diabetes, maintaining stable blood sugar levels is challenging. GLP-1 medications help in several ways:
- Enhancing glucose-dependent insulin secretion: GLP-1 medications increase insulin production in response to increased blood sugar, helping to prevent postprandial hyperglycemia (blood sugar spikes after meals) without causing hypoglycemia (dangerously low blood sugar).
- Suppressing glucagon: By reducing the amount of glucagon – a hormone that signals the liver to release stored sugar into the blood – GLP-1 medications help prevent the liver from releasing too much sugar into the bloodstream and help prevent blood sugar spikes after meals.
- Slowing gastric emptying: This process helps slow the absorption of sugar and prevent rapid blood sugar increases after eating, stabilizing blood sugar control
GLP-1 medications, such as Ozempic and Mounjaro, are effective in reducing HbA1c levels (a key measure of long-term blood sugar control) and help reduce the risk of complications associated with Type 2 diabetes.
2. Curbs Hunger and Food Noise
GLP-1 medications, including Wegovy and Saxenda, have been approved for weight loss in people who are obese or overweight. Studies also found that GLP-1 medications were effective in promoting weight loss when used alongside a healthy diet and exercise program. These medications promote weight loss by:
- Suppressing appetite: GLP-1 medications act on the brain’s hypothalamus to reduce hunger signals, helping individuals reduce cravings and eat fewer calories.
- Promoting satiety: Slower gastric emptying, the rate at which food leaves your stomach. This prolongs feelings of fullness, reducing the urge to snack between meals and lowering calorie intake.
- Increasing energy expenditure: Some studies suggest that GLP-1 medications may increase calorie burning and regulate fat metabolism, further aiding weight loss through these metabolic effects.
For people who have found it difficult to lose weight despite dieting and exercising, GLP-1 medications can provide additional support.
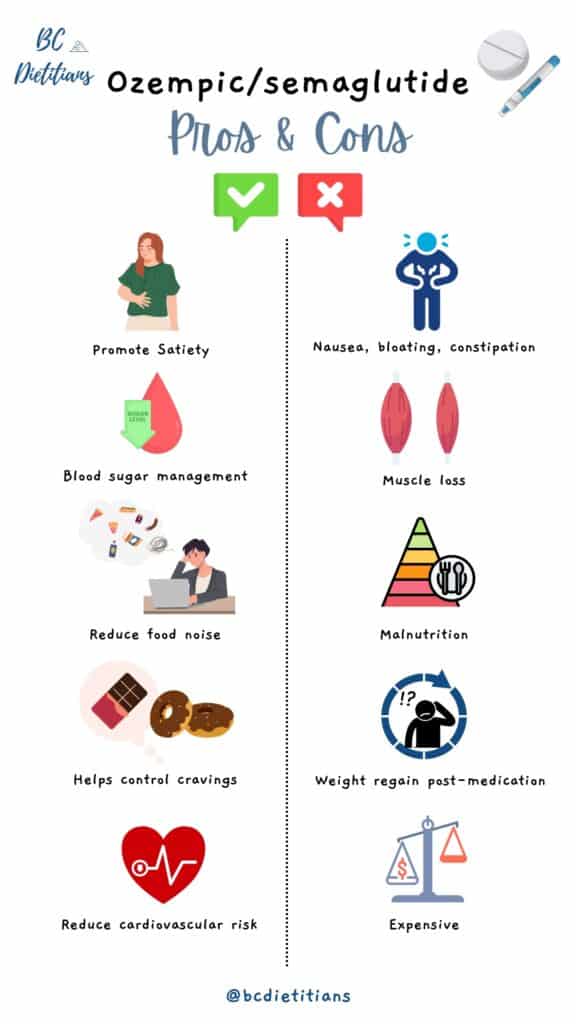
The Long-Term Impact of GLP-1 Medications: Sustainability and Maintenance
While GLP-1 medications can help individuals achieve significant weight loss and improve blood sugar regulation in the short term, the long-term sustainability of these benefits largely depends on continued lifestyle changes and medication. These medications are meant to be used long-term to sustain the benefits.
Many individuals see GLP-1 medications as a quick fix for weight loss, overlooking the crucial role of diet and exercise. If GLP-1 medications are stopped, specially without incorporating sustainable lifestyle changes, you will experience weight regain of fat tissues. Research showed that weight regain is common after discontinuing semaglutide (a common GLP-1 medication), with participants regaining two-thirds of the weight they lost, and improvements in risk factors like blood pressure and HbA1c also reversed.
Therefore, it’s important to create and maintain personalized, long-term strategies that focus on behavioral changes and mindset shifts before, during, and after stopping GLP-1 medications. Dietitians are essential in helping clients maintain a healthy, balanced approach to weight management that doesn’t rely on quick fixes like medications alone. We highly recommend consulting with a BC dietitian before starting GLP-1 medications so that we can provide you with personalized advice that aligns with your goals and treatment plan.
Side Effects
GLP-1 medications can cause a range of side effects, most commonly gastrointestinal issues such as nausea, vomiting, diarrhea, constipation, and dizziness. However, these side effects can often be mitigated with personalized nutrition. Here’s how your diet can help manage potential side effects:
1. Gut Discomfort (Nausea, Vomiting, Diarrhea)
These issues can be minimized with a high-fiber diet that includes fruits, vegetables, whole grains, and lean proteins, which support digestive health and prevent constipation.
2. Headaches, Dizziness, and Fatigue
These are often due to dehydration, blood sugar fluctuations, or even caffeine withdrawal. Drinking plenty of water, avoiding caffeine spikes, and eating regular meals that balance carbohydrates, proteins, and healthy fats can help stabilize blood sugar levels, provide sustained energy levels, and avoid nutrient deficiencies.
3.Muscle Loss
Muscle loss may occur, especially with insufficient protein intake. Ensure your diet includes adequate lean proteins (like chicken, tofu, and fish) and consider strength training to preserve muscle mass and support your metabolism and overall health.
4. Bone Density Loss
GLP-1 medications may affect bone health, so calcium and vitamin D intake is important. Incorporate dairy products, leafy greens, and fortified foods to support bone strength.
This review article emphasized the importance of a balanced diet to reduce the risk of adverse health outcomes and improve the effectiveness of diabetes medications like GLP-1.
Overcoming Challenges and Common Mistakes with GLP-1 Medications
While GLP-1 medications are effective, they do come with challenges:
- Gastrointestinal issues: Common side effects include nausea and constipation. These can make it difficult to eat enough, especially protein, and maintain proper nutrition.
- Reduced appetite: GLP-1 medications can result in a lack of interest in food, potentially leading to undereating, causing nutrient deficiencies and potential muscle loss.
- Bone and muscle loss: The combination of reduced appetite and weight loss can lead to reduced muscle mass and bone density over time, especially when paired with inadequate protein intake and absence of strength training.
Common mistakes include:
- Skipping meals: Many users might skip meals due to reduced appetite, thinking it will help them lose more weight. However, eating too little can exacerbate muscle loss, fatigue, and nutrient deficiencies. It’s essential to maintain a balanced diet to support overall health and prevent energy imbalances, even while managing appetite suppression with GLP-1 medications.
- Not prioritizing protein intake: Lack of protein intake can lead to further muscle loss.
- Dehydration: GLP-1 medications and potential side effects can contribute to dehydration, so adequate water intake is essential.
Over time, adjusting to a healthy, balanced diet and ensuring proper hydration can help overcome these challenges, avoid pitfalls, and maximize the benefits of GLP-1 medications. Combine these medications with personalized nutrition, strength training, and regular health monitoring to create a sustainable, healthy lifestyle that supports your long-term goals.
Key Takeaway: The Importance of Personalized Nutrition
To maximize the effectiveness of GLP-1 medications and minimize side effects, personalized nutrition is critical to align with the goals of the medication. A tailored diet plan should include:
- Nutrient-dense foods that provide energy without excess calories.
- Adequate vitamins and minerals.
- Adequate protein to preserve muscle mass.
- Low-glycemic foods that support stable blood sugar levels.
- Foods that are tailored to individual needs and preferences.
By collaborating with a registered dietitian, you can create a personalized nutrition plan that supports weight loss and blood sugar control while addressing the unique challenges of GLP-1 medication use.
GLP-1 medications can be beneficial for managing Type 2 diabetes and promoting weight loss in some people, but they may not be suitable for everyone. It’s important to consult with your healthcare provider to determine if they’re right for you. GLP-1 medications work best when combined with a balanced diet, regular exercise, and sustainable lifestyle habits.
If you’re considering GLP-1, consulting a registered dietitian can help you optimize the benefits, manage side effects, and develop a sustainable plan tailored to your health goals. Healthcare professionals can guide you through the process, ensuring a comprehensive approach that supports long-term success.
Blog Contributors:
Amy Chow, Registered Dietitian
Eileen Huang, BSc. Food, Nutrition, and Health
References
Brunton, S. A., & Wysham, C. H. (2020). GLP-1 receptor agonists in the treatment of type 2 diabetes: role and clinical experience to date. Postgraduate Medicine, 132(sup2), 3–14. https://www.tandfonline.com/doi/full/10.1080/00325481.2020.1798099
Bu, T., Sun, Z., Pan, Y., et al. (2024). Glucagon-Like Peptide-1: New Regulator in Lipid Metabolism. Diabetes & Metabolism Journal, 48(3), 354–372. https://www.e-dmj.org/journal/view.php?doi=10.4093/dmj.2023.0277
Collins L, Costello RA. Glucagon-Like Peptide-1 Receptor Agonists. [Updated 2024 Feb 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. https://www.ncbi.nlm.nih.gov/books/NBK551568/
Deane, A. M., Nguyen, N. Q., Stevens, J. E., et al. (2010). Endogenous glucagon-like peptide-1 slows gastric emptying in healthy subjects, attenuating postprandial glycemia. The Journal of clinical endocrinology and metabolism, 95(1), 215–221. https://pubmed.ncbi.nlm.nih.gov/19892837/
Drucker, Daniel J. (2018). Mechanisms of Action and Therapeutic Application of Glucagon-like Peptide-1. Cell Metabolism, Volume 27, Issue 4, 740 – 756. https://www.sciencedirect.com/science/article/pii/S1550413118301797
Gorgojo-Martínez, J. J., Mezquita-Raya, P., Carretero-Gómez, J., et al. (2022). Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus. Journal of clinical medicine, 12(1), 145. https://pmc.ncbi.nlm.nih.gov/articles/PMC9821052/
J.P. Morgan Research (2023). The increase in appetite for obesity drugs. Retrieved from: https://www.jpmorgan.com/insights/global-research/current-events/obesity-drugs
Lundgren, J. R., Janus, C., Jensen, S. B. K., et al. (2021). Healthy Weight Loss Maintenance with Exercise, Liraglutide, or Both Combined. The New England journal of medicine, 384(18), 1719–1730. https://pubmed.ncbi.nlm.nih.gov/33951361/
Pirro, V., Roth, K. D., Lin, Y., et al. (2022). Effects of Tirzepatide, a Dual GIP and GLP-1 RA, on Lipid and Metabolite Profiles in Subjects With Type 2 Diabetes. The Journal of clinical endocrinology and metabolism, 107(2), 363–378. https://pubmed.ncbi.nlm.nih.gov/34608929/
Popoviciu, M. S., Păduraru, L., Yahya, G., et al. (2023). Emerging Role of GLP-1 Agonists in Obesity: A Comprehensive Review of Randomised Controlled Trials. International journal of molecular sciences, 24(13), 10449. https://doi.org/10.3390/ijms241310449
Trujillo, J. M., Nuffer, W., & Smith, B. A. (2021). GLP-1 receptor agonists: an updated review of head-to-head clinical studies. Therapeutic advances in endocrinology and metabolism, 12, 2042018821997320. https://pmc.ncbi.nlm.nih.gov/articles/PMC7953228/
Viljoen, A., Bain, S. C. (2023). Glucagon-Like Peptide 1 Therapy: From Discovery to Type 2 Diabetes and Beyond. Endocrinology and Metabolism, 38(1), 25–33. https://www.e-enm.org/journal/view.php?doi=10.3803/EnM.2022.1642
Wadden TA, Bailey TS, Billings LK, et al. (2021). Effect of Subcutaneous Semaglutide vs Placebo as an Adjunct to Intensive Behavioral Therapy on Body Weight in Adults With Overweight or Obesity: The STEP 3 Randomized Clinical Trial. JAMA, 325(14), 1403–1413. https://pmc.ncbi.nlm.nih.gov/articles/PMC7905697/
Wilding JPH, Batterham RL, Davies M, et al. (2022). Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022; 24(8): 1553-1564. doi:10.1111/dom.14725. https://dom-pubs.onlinelibrary.wiley.com/doi/10.1111/dom.14725









Add a comment