Endometriosis is a complex, inflammatory condition that affects an estimated 1 in 10 women, yet it often goes undiagnosed for years. Many people are told their symptoms are simply part of having a menstrual cycle. Endometriosis can affect far more than just the pelvis because of this its signs are frequently misattributed to digestive disorders or other potential conditions.
Understanding when symptoms warrant further investigation is a critical step toward earlier diagnosis, appropriate care, and improved quality of life.
Below are some of the most common signs that may suggest endometriosis is worth considering, especially if symptoms are persistent, worsening, or interfering with daily life.

Samantha Thompson, Registered Dietitian and Integrative & Functional Nutrition Certified Practitioner
1. Pain is one of the most prominent symptoms of endometriosis
Pain affects up to 90% of patients with endometriosis (Nnoaham et al., 2011).
The pain, which often manifests as dysmenorrhea (painful menstruation), can also occur during ovulation and may be constant or intermittent throughout the cycle. Patients frequently report discomfort during activities such as sexual intercourse (dyspareunia) or during bowel movements.
The pathophysiology behind this vast array of pain symptoms lies in the proliferation of sensory nerve fibers within endometrial lesions, which can alter pain pathways and heighten sensitivity in an inflammatory environment (Vigano et al., 2015).
This abnormal nerve growth leads to the phenomenon known as “central sensitization,” where pain perception is amplified, significantly impacting quality of life.
2. Digestive issues and IBS symptoms
Digestive complications are prevalent in individuals with endometriosis, with studies revealing that approximately 30% to 40% are diagnosed with irritable bowel syndrome (IBS) (Khan et al., 2015).
The overlapping symptoms of IBS and endometriosis, including bloating, gas, and abdominal pain, can complicate diagnosis and treatment.
Moreover, a subset of patients may develop small intestinal bacterial overgrowth (SIBO), conditions which may arise due to endometrial lesions obstructing normal intestinal function (Fitzgerald et al., 2019). Research demonstrates that SIBO can lead to adverse gastrointestinal symptoms and worsen overall patient well-being.
3. Chronic fatigue
Chronic fatigue syndrome (CFS) is a debilitating condition often reported by up to 60% of women with endometriosis, which can severely impact daily functioning (Levy et al., 2016).
Factors contributing to this fatigue include persistent pelvic pain, sleep disturbances, and the body’s ongoing inflammatory response to the disease (Takahashi et al., 2020).
Unlike typical fatigue that may resolve with rest, CFS can lead to significant limitations in one’s ability to perform everyday activities, highlighting the need for comprehensive management strategies.
4. Hormone imbalance and thyroid dysfunction
Hormonal imbalances are frequently observed in patients with endometriosis, with research suggesting that dysregulation among thyroid, adrenal, and sex hormones is common (Pérez-López et al., 2016).
A study found that women with endometriosis had significantly altered levels of estradiol and progesterone, which can exacerbate the disease’s symptoms and contribute to lesion growth.
One intriguing aspect is known as progesterone resistance. Even when progesterone is present in the body, it may not function effectively due to various factors such as genetic transcription issues, epigenetic changes, or the influence of microRNAs.
This resistance can lead to the persistence of lesions while an imbalance often tilts toward excessive estrogen activity, which can further aggravate the condition (Horne & Laird, 2019; Giudice & Kao, 2004).
Additionally, thyroid dysfunction has been associated with endometriosis, impacting overall health and potentially complicating treatment strategies (Odeh et al., 2019).
5. Fertility Challenges
Fertility issues are a significant concern for women with endometriosis, with estimates indicating that approximately 30-40% of affected individuals may struggle to conceive (Agarwal et al., 2019).
The presence of endometrial lesions can disrupt ovarian function and alter hormonal signaling, leading to reproductive challenges.
It is recommended that women who have been attempting to conceive for over a year consult a specialist to evaluate for endometriosis, as effective treatment of the disease can enhance fertility outcomes (Kozlowski et al., 2021).
6. Depression and Anxiety
Mental health challenges are common among individuals diagnosed with endometriosis.
A systematic review found that nearly 50% of women with endometriosis reported experiencing anxiety or depression, with studies suggesting that chronic pain and the stress of managing a significant health issue contribute to this mental health burden (Horne et al., 2020).
Furthermore, suicidal ideation is significantly more prevalent in this population, underlining the critical need for mental health support alongside physical treatment for endometriosis.
7. Autoimmune diseases
Individuals with endometriosis often present with immune dysfunction, leading to an increased incidence of allergies and autoimmune diseases.
Research indicates that around 25% of women with endometriosis may develop an autoimmune condition, which may be exacerbated by systemic inflammation (Gonzalez et al., 2020).
The dysregulation of immune responses is believed to contribute to the persistence and severity of endometrial lesions, further complicating the clinical picture.
Summary
Endometriosis is a systemic condition involving inflammation, immune dysfunction, hormonal signaling, and nervous system sensitization, which is why symptoms often extend well beyond the pelvis. In the presence of multiple or worsening symptoms, consultation with a healthcare professional is recommended.
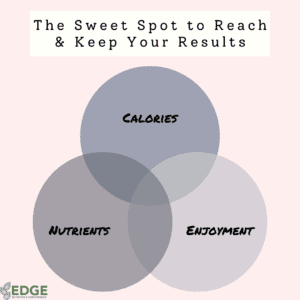
While diagnosis and medical management are essential, nutrition can play a meaningful supportive role in endometriosis care.
An evidence-informed nutrition approach can help reduce inflammatory burden, support gut and immune health, stabilize blood sugar, and address nutrient deficiencies that commonly worsen pain, fatigue, mood symptoms, and digestive distress.
If you suspect endometriosis or are navigating a diagnosis, working with a registered dietitian who understands the condition can help you cut through conflicting advice, avoid unnecessary eliminations, and build a sustainable plan alongside your medical care team.
Earlier recognition and a multidisciplinary approach can make a real difference in symptom control and quality of life.





Add a comment